For decades, vasectomy has been a reliable form of permanent contraception for men. Among the surgical variations available, the No Scalpel Vasectomy (NSV) has become the gold standard due to its minimally invasive nature, reduced recovery time, and lower complication rates. However, an important question that often arises among men considering the procedure is whether a no scalpel vasectomy affects their hormonal balance.
Since hormones such as testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) play a central role in sexual health, energy levels, and overall wellbeing, the relationship between no scalpel vasectomy and hormonal equilibrium warrants careful analysis.
This article explores the scientific evidence surrounding hormonal changes (or the lack thereof) after no scalpel vasectomy, examining both clinical findings and theoretical mechanisms. It will also discuss long-term health considerations, psychological factors, and patient-reported outcomes to give a complete picture of how NSV interacts with the male endocrine system.
Table of Contents
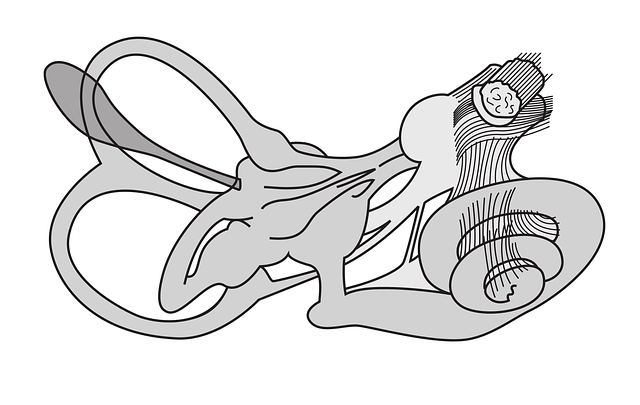
Unlike traditional vasectomy, which involves incisions and sutures, a No Scalpel Vasectomy uses a small puncture made with specialized instruments. Through this puncture, the surgeon isolates, cuts, and seals the vas deferens—the tubes that transport sperm from the testes to the urethra.
- Key point: The testes remain intact and continue producing sperm.
- Hormone production is unaffected because the Leydig cells in the testes, responsible for testosterone secretion, are not disturbed by the surgery.
- The pituitary hormones (LH and FSH), which regulate testicular function, also continue their work as usual.
Thus, the surgical approach itself does not directly interfere with endocrine activity.
Also Read: Premium Software Boxes for Digital and Retail Packaging
One of the most common concerns men express before vasectomy is whether testosterone will decline.
- Large-scale studies have consistently shown no significant change in serum testosterone levels after no scalpel vasectomy.
- A 2018 meta-analysis reviewing over 25 studies concluded that men undergoing vasectomy (including NSV) did not experience measurable reductions in testosterone, even decades after the procedure.
- Some studies even suggest a slight compensatory rise in testosterone due to reduced sperm utilization, but these findings remain inconsistent.
Testosterone is produced in the testes under the control of LH. Since NSV only blocks the passage of sperm and does not disrupt Leydig cells or pituitary regulation, there is no physiological reason for testosterone production to decrease.
Conclusion: No scalpel vasectomy does not impair testosterone production or circulation.
To fully assess hormonal equilibrium, it is essential to look beyond testosterone.
- LH drives Leydig cells to produce testosterone.
- Multiple longitudinal studies demonstrate no disruption of LH secretion post-NSV.
- FSH regulates sperm development in the testes.
- After NSV, sperm production continues, but the sperm are reabsorbed within the testes or epididymis.
- FSH levels generally remain stable, indicating no feedback loop disturbance.
- Though less central in male reproductive function, prolactin can influence libido and psychological wellbeing.
- No correlation has been found between vasectomy (scalpel or no scalpel) and elevated prolactin levels.
A related concern is whether changes in hormones after NSV might affect sexual desire.
- Studies indicate libido is maintained or even improved after vasectomy.
- Improvements often stem from psychological relief—men no longer worry about unintended pregnancies.
- Since testosterone and related hormones are unaffected, the biological basis for libido remains intact.
Interestingly, while objective hormone levels remain stable, some men report subjective symptoms such as fatigue, reduced sex drive, or mood shifts post-vasectomy.
- Psychological adjustment – A vasectomy, even with the minimally invasive NSV method, represents a major life decision that can trigger subconscious stress or regret.
- Age-related changes – Men who undergo vasectomy in their 30s or 40s may begin to naturally experience subtle testosterone decline, which might be mistakenly attributed to the surgery.
- Misinformation – Persistent myths about vasectomy affecting masculinity or hormones may amplify perceived changes.
Research on the relationship between vasectomy and prostate cancer has been inconclusive. Importantly, hormonal disruption is not a suspected mechanism. Current guidelines do not list NSV as a risk factor for prostate issues.
Since testosterone regulates muscle mass, fat distribution, and energy levels, any change in hormonal equilibrium could theoretically affect metabolism. Studies show no significant metabolic shifts attributable to NSV.
There is limited evidence suggesting vasectomy may increase the production of antisperm antibodies. While this is an immunological rather than hormonal effect, it does not appear to impact testosterone, LH, or FSH levels.
- No Scalpel Vasectomy causes less trauma to surrounding tissue.
- Reduced inflammation may theoretically lower risks of subtle testicular stress compared to traditional vasectomy.
- However, both approaches have been shown not to alter hormone production.
Clinicians often report that patients express initial worry about hormone levels, especially testosterone. However, follow-up evaluations typically confirm normal hormonal balance.
Example case:
- A 42-year-old man underwent NSV and later reported concerns about decreased energy. Lab results showed testosterone and LH within normal ranges. His fatigue was eventually linked to lifestyle factors rather than the vasectomy.
While decades of studies have reassured men about hormonal safety, emerging technologies such as genomic analysis and proteomics may uncover subtle molecular changes post-vasectomy. Future areas of investigation may include:
- Epigenetic changes in testicular gene expression.
- Long-term endocrine interactions with immune responses.
- Differentiating age-related testosterone decline from surgical outcomes.
The overwhelming consensus from clinical evidence is clear: No Scalpel Vasectomy does not disrupt hormonal equilibrium. Testosterone, LH, FSH, and prolactin remain stable after the procedure. Men can expect to maintain their sexual function, vitality, and overall hormonal balance post-NSV.
The only “changes” men may notice are psychological or age-related, rather than caused by the procedure itself. For those considering vasectomy, the no scalpel technique provides a safe, effective, and minimally invasive option with no risk of hormonal imbalance.
1. Does a no scalpel vasectomy lower testosterone?
No. Clinical studies consistently show that testosterone levels remain stable after no scalpel vasectomy. The procedure does not affect the Leydig cells that produce testosterone.
2. Can a no scalpel vasectomy affect sex drive or performance?
No scalpel vasectomy does not biologically reduce libido or sexual performance. In fact, many men report improved sexual satisfaction due to reduced anxiety about pregnancy.
3. Are there any long-term hormonal risks with no scalpel vasectomy?
No significant long-term hormonal risks have been identified. Hormone levels such as testosterone, LH, and FSH remain within normal ranges decades after the procedure.